- Bicornuate Uterus vs Septate Uterus: Definitions, Similarities, and Differences
- Bicornuate Uterus: In-depth Analysis
- Septate Uterus: Unveiling the Details
- Clinical Presentation and Symptoms
- Overlapping Symptoms and Challenges in Diagnosis
- Reproductive Implications
- Risk of Miscarriages and Preterm Births in Septate Uterus Cases
- Medical Management
- Surgical Intervention
- Future Fertility Trends and Innovations
- CONCLUSION
- FAQS
Welcome to an insightful journey into the realm of reproductive health. If you’ve ever wondered about the intricate differences between a bicornuate uterus and a septate uterus, you’re in the right place. We understand that navigating these medical terms and understanding their impact can be overwhelming. But worry not, as we’re here to shed light on these two conditions and guide you toward informed decisions about your well-being.
Bicornuate Uterus vs Septate Uterus: Definitions, Similarities, and Differences
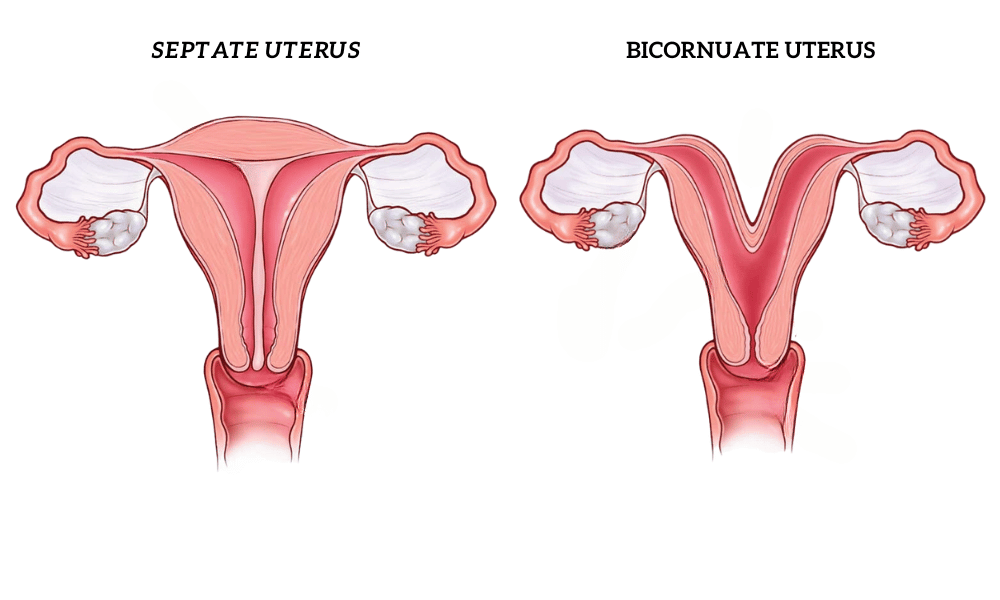
A bicornuate uterus and a septate uterus are both types of Müllerian duct anomalies, which are congenital abnormalities of the female reproductive tract that occur when the Müllerian ducts fail to develop normally.
Bicornuate Uterus: A bicornuate uterus is heart-shaped, with a deep indentation at the top. This condition occurs when the two ducts that form the uterus fail to fuse completely during fetal development1.
Septate Uterus: A septate uterus has a normal outer shape, but there is a wall of tissue (septum) that divides the interior of the uterus into two cavities. This condition occurs when the tissue that lines the uterus (endometrium) invades the muscular wall of the uterus (myometrium)2.
Both conditions can be asymptomatic, meaning they don’t always cause noticeable symptoms. Some women may not even realize they have these conditions until they undergo imaging tests for other reasons.
Bicornuate Uterus: In-depth Analysis
Definition and Characteristics of a Bicornuate Uterus
A bicornuate uterus, also known as a “heart-shaped” uterus, is a type of congenital Müllerian duct anomaly where the uterus has two horns and a deep indentation at the top. This condition occurs when the two ducts that form the uterus fail to merge completely during fetal development1.
The bicornuate uterus can range in severity depending on how much the uterus is divided. It’s typically characterized by a normal cervical and vaginal anatomy with an abnormal uterine fundus, the top portion of the uterus.
Types of Bicornuate Uterus Based on Severity
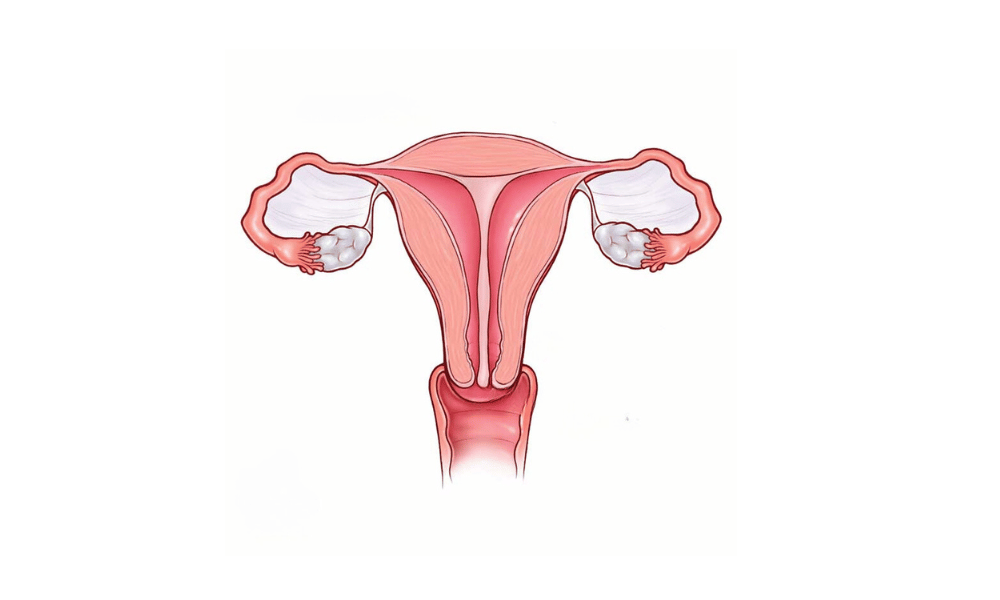
The severity of a bicornuate uterus is generally classified into two types:
- Bicornuate Unicollis: This condition is characterized by a uterus with two cavities and one cervix. The outer surface of the uterus appears normal, but the interior is divided by a wall that extends into the uterus from the top.
- Bicornuate Bicollis: This is a more severe form where the uterus has two cavities and two cervices. This means that each half of the uterus has its own cervix, leading to the vagina2.
Developmental Causes and Theories
The exact cause of a bicornuate uterus is not known, but it is believed to result from abnormal embryological development. Specifically, it occurs when the Müllerian ducts fail to fuse properly during fetal development, resulting in a uterus that is divided into two horns3. Genetic factors may play a role, but the condition is usually sporadic and not inherited.
Diagnostic Methods for Identifying a Bicornuate Uterus
Diagnosis of a bicornuate uterus can be challenging because the external shape of the uterus often appears normal. However, several imaging techniques can help identify this condition:
- Ultrasound: This is often the first step in diagnosis. A transvaginal ultrasound can provide detailed images of the uterus and may reveal the characteristic heart-shaped appearance of a bicornuate uterus.
- Magnetic Resonance Imaging (MRI): This provides a more detailed view of the uterus and can help differentiate a bicornuate uterus from other types of Müllerian duct anomalies4.
- Hysterosalpingography (HSG): This is a special type of X-ray used to examine the uterus and fallopian tubes. It can help identify the presence of a septum or other abnormalities in the uterus5.
- Hysteroscopy: This procedure allows the doctor to look inside the uterus with a small, lighted instrument. It can provide a direct view of the internal structure of the uterus6.
Septate Uterus: Unveiling the Details
Definition and Features of a Septate Uterus
A septate uterus is a type of congenital Müllerian duct anomaly characterized by a normal uterine shape on the outside but a wall of tissue (septum) dividing the interior of the uterus into two cavities. This condition occurs when the tissue that lines the uterus (endometrium) invades the muscular wall of the uterus (myometrium)1.
A septate uterus does not typically affect the appearance of the external uterine structure, but it can have significant implications for fertility and pregnancy outcomes.
Distinction Between Complete and Partial Septate Uterus
The severity of a septate uterus is generally classified into two types:
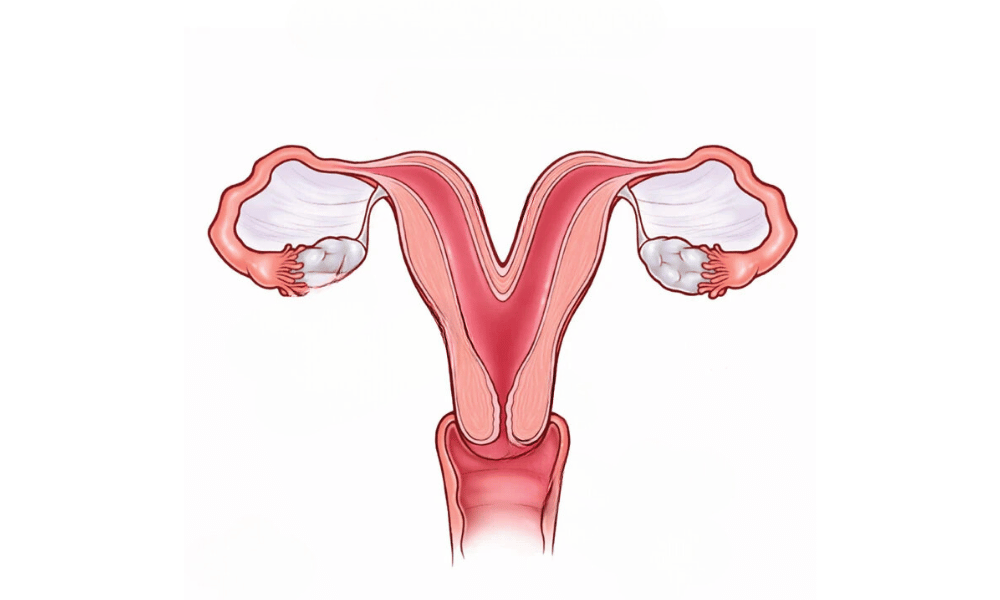
- Complete Septate Uterus: In this condition, the septum extends from the top of the uterus down to the cervix, fully dividing the uterine cavity into two separate spaces.
- Partial Septate Uterus: In this less severe form, the septum does not reach as far down and only partially divides the uterine cavity2.
Embryological Origins and Predisposing Factors
A septate uterus arises from an error during embryonic development. Normally, the two Müllerian ducts fuse together to form a single uterine cavity, and the septum between them breaks down. In a septate uterus, this resorption process is incomplete, leaving a wall of tissue within the uterus3.
The exact cause of this developmental abnormality is still unknown, but research suggests that genetic factors may play a role4. It is not typically associated with any other syndrome or genetic condition and usually occurs sporadically.
Diagnostic Techniques for Identifying a Septate Uterus
Several imaging techniques can be used to diagnose a septate uterus:
- Ultrasound: A transvaginal ultrasound can provide a preliminary diagnosis by visualizing the septum within the uterus.
- Magnetic Resonance Imaging (MRI): MRI provides a more detailed view of the uterus and can help differentiate a septate uterus from other types of Müllerian duct anomalies5.
- Hysterosalpingography (HSG): This X-ray procedure can reveal the presence of a septum within the uterus6.
Hysteroscopy: This procedure allows doctors to view the inside of the uterus directly and can provide a definitive diagnosis7
Clinical Presentation and Symptoms
Symptoms Associated with Bicornuate Uterus
A bicornuate uterus may not cause any noticeable symptoms in some women. However, when symptoms do occur, they can include:
- Recurrent Miscarriages: Women with a bicornuate uterus have a higher risk of miscarriage due to the abnormal shape of the uterus.
- Preterm Birth: The irregular shape of the uterus can also lead to preterm birth, as it may not provide enough space for the baby to grow to full term1.
- Abnormal Positioning of the Fetus: The baby may not position itself head-down before birth, leading to breech or transverse presentations1.
Symptoms Associated with Septate Uterus
Like a bicornuate uterus, a septate uterus may be asymptomatic in some women. However, potential symptoms can include:
- Recurrent Miscarriages: Women with a septate uterus have an increased risk of recurrent miscarriage, especially in the first trimester. This is because the septum does not have the same blood supply as the rest of the uterus, making it difficult for an embryo to implant or for a fetus to grow2.
Overlapping Symptoms and Challenges in Diagnosis
While both conditions can lead to recurrent miscarriages, they are distinct entities with different anatomical features. However, the overlapping symptoms can make diagnosis challenging. Furthermore, many women with these conditions do not experience any symptoms until they try to conceive, which can delay diagnosis.
Differentiating between a bicornuate uterus and a septate uterus is crucial because the management and treatment strategies differ for each condition. Imaging techniques such as ultrasound, MRI, and hysteroscopy play a vital role in accurately diagnosing these conditions3.
Reproductive Implications
Impact of Bicornuate Uterus on Fertility
A bicornuate uterus is a rare anomaly and it’s associated with worse reproductive outcomes. However, it doesn’t significantly affect a woman’s ability to conceive1. Most women with a bicornuate uterus have no extra difficulties with conception2. Yet, it’s noteworthy that about 1 percent of women with infertility have a bicornuate uterus3.
Pregnancy Complications Linked to Bicornuate Uterus
While fertility may not be largely affected, a bicornuate uterus can cause complications during pregnancy. These can include recurrent pregnancy loss and preterm labor1. The irregular shape of the uterus can also lead to abnormal positioning of the fetus such as breech or transverse presentations4.
Influence of Septate Uterus on Conception
A septate uterus, unlike a bicornuate uterus, has been directly associated with recurrent miscarriages and infertility. The septum within the uterus has a poor blood supply, which can make it difficult for an embryo to implant or for a fetus to grow, thus affecting conception5.
Risk of Miscarriages and Preterm Births in Septate Uterus Cases
Women with a septate uterus have an increased risk of miscarriage, especially in the first trimester5. This is likely due to the poor vascularization of the septum, which can prevent the embryo from receiving the nutrients it needs to develop. In addition to an increased risk of miscarriage, women with a septate uterus may also have a higher risk of preterm birth6.
Risks and Complications
Both a bicornuate uterus and a septate uterus can affect a woman’s fertility and pregnancy outcomes, but the risks and complications associated with each condition are slightly different.
Bicornuate Uterus: Women with a bicornuate uterus have a higher risk of miscarriage and preterm birth. The abnormal shape of the uterus can also lead to malpresentation (such as breech or transverse presentation), where the baby is not positioned head-down in the womb before birth3.
Septate Uterus: Women with a septate uterus have an increased risk of recurrent miscarriage, mainly in the first trimester. The septum does not have the same blood supply as the rest of the uterus, which can make it difficult for an embryo to implant or for a fetus to grow4.
Medical Management
Non-surgical Approaches for Managing Uterine Anomalies
While surgical intervention may be necessary in some cases of uterine anomalies, non-surgical approaches are often preferable due to lower risk and less physical trauma. These can include watchful waiting, hormonal treatments, or the use of assisted reproductive technologies.
For example, in the case of uterine fibroids, non-surgical approaches such as uterine artery embolization can be effective. This procedure involves blocking the blood supply to the fibroids, causing them to shrink1.
Hormonal Treatments and Their Effectiveness
Hormonal treatments can sometimes be used to manage symptoms of uterine anomalies. For instance, hormonal contraceptives can help regulate menstrual cycles and reduce heavy bleeding associated with certain uterine anomalies2.
However, the effectiveness of hormonal treatments can vary depending on the specific anomaly and the individual patient’s response to treatment. As such, it’s essential to discuss these options with a healthcare provider.
Role of Assisted Reproductive Technologies (ART) in Overcoming Fertility Issues
Assisted Reproductive Technologies (ART), such as in-vitro fertilization (IVF) or intrauterine insemination (IUI), can play a crucial role in helping women with uterine anomalies achieve pregnancy. These technologies can bypass certain obstacles to natural conception, such as problems with embryo implantation that can occur in a septate uterus3.
Surgical Intervention
Surgical Options for Correcting Uterine Anomalies
Surgical correction is often considered for women with uterine anomalies who experience symptoms or complications. The choice of procedure depends on the type of uterine anomaly.
- Hysteroscopic Metroplasty: This minimally invasive procedure is commonly used to correct a septate uterus. It involves resecting the septum to create a normal uterine cavity12.
- Laparoscopy: Laparoscopic surgery can be used to correct various uterine anomalies, including a bicornuate or unicornuate uterus3. It’s a minimally invasive approach that uses small incisions and a camera to guide the surgery.
- Robotic-Assisted Surgery: This advanced technique provides greater precision and control during surgery, making it useful for complex uterine anomalies4.
Resection of Septum in Septate Uterus Cases
For women with a septate uterus, hysteroscopic metroplasty is the standard treatment. This procedure involves using a hysteroscope, a thin tube with a light and camera, to visualize the uterus. The septum is then cut and removed, leaving a normal uterine cavity. This procedure can significantly improve pregnancy outcomes for women with a history of recurrent miscarriages5.
Surgical Challenges and Considerations
While surgical correction of uterine anomalies can significantly improve reproductive outcomes, these procedures are not without challenges.
The complexity of the anomaly, patient’s health status, and surgical skills are all factors that can impact the success of the procedure6. Furthermore, there are risks associated with any surgery, such as infection, bleeding, and damage to surrounding organs. Therefore, the decision to pursue surgical intervention should be made after careful consultation with a healthcare provider
Future Fertility Trends and Innovations
Research Advancements in Uterine Anomaly Treatments
Recent research has contributed significantly to the understanding and management of uterine anomalies. For instance, advancements have been made in the diagnosis and treatment of dysfunctional uterine bleeding1.
There’s also a growing body of research on the etiology of uterine fibroids, which are common non-cancerous growths that can alter the shape of the uterus and potentially impact fertility2.
Moreover, studies are exploring new treatment options for recurrent spontaneous abortion, a condition often associated with uterine anomalies3.
Emerging Technologies and Their Potential Impact
Emerging technologies hold great promise in the field of reproductive medicine. For example, hysteroscopy is a technique that allows doctors to view the inside of the uterus and treat various conditions. Research is underway to determine its effectiveness in treating subfertility associated with suspected major uterine cavity abnormalities4.
Furthermore, modern imaging techniques such as MRI have greatly improved the diagnosis of Müllerian anomalies, which include a range of congenital uterine abnormalities5.
Hope for Improved Outcomes in the Future
With ongoing advances in research and technology, there’s hope for improved outcomes for women with uterine anomalies. As our understanding of these conditions improves, so too will our ability to effectively manage them and mitigate their impact on fertility and pregnancy outcomes.
CONCLUSION
I hope the Bicornuate Uterus vs Septate Uterus comparison have clear all your questions. while a bicornuate uterus and a septate uterus are both congenital abnormalities of the female reproductive system, they have distinct characteristics and implications for pregnancy and fertility. Understanding these conditions can help women make informed choices about their reproductive health.
YOU MAY ALSO LIKE:
- Exploring the Myomatous Uterus: A Comprehensive Guide
- How to heal scar tissue in uterus naturally : A Holistic Guide for Natural Healing.
- Comprehensive Guide on How to clean uterus after a miscarriage naturally at home
- Understanding and Managing Stabbing pain in uterus
FAQS
What is the primary difference between bicornuate and septate uteri?
Bicornuate Uterus: A bicornuate uterus is characterized by a uterus that has two distinct horn-like structures, giving it a heart-shaped appearance. This occurs due to incomplete fusion of the Müllerian ducts during fetal development.
Septate Uterus: A septate uterus, on the other hand, appears externally normal but has a septum or a wall of tissue that divides the uterine cavity partially or completely. This septum results from the incomplete resorption of tissue that forms during fetal development.
How are uterine anomalies diagnosed?
Ultrasound: Transvaginal ultrasound can provide clear images of the uterus, helping to identify structural abnormalities.
Hysterosalpingography (HSG): This involves injecting a contrast material into the uterus and taking X-rays to visualize the uterine cavity and fallopian tubes.
Hysteroscopy: A thin, lighted tube (hysteroscope) is inserted through the vagina and cervix to directly visualize the uterine cavity.
MRI (Magnetic Resonance Imaging): MRI can provide detailed images of the uterine structure and is particularly useful for complex cases.
Can pregnancy be achieved naturally with these anomalies?
What are the challenges associated with surgical correction?
Complexity: Surgical correction can be intricate, especially in cases where the abnormality involves a delicate removal of tissue or reconstruction of the uterine structure.Risks: Any surgical procedure carries inherent risks, including infection, bleeding, and anesthesia-related complications.
Fertility Impact: Surgical correction might not always guarantee improved fertility outcomes. In some cases, the surgery itself can lead to scarring and adhesions that affect fertility.
Recovery: Recovery following surgery can vary, and some procedures might require a longer healing period.
Future Pregnancy: While surgical correction can improve pregnancy outcomes, there is no absolute guarantee of a complication-free pregnancy afterward.
How do emotional factors affect individuals dealing with uterine anomalies?
Stress and Anxiety: The uncertainty surrounding fertility and pregnancy outcomes can lead to stress and anxiety.
Body Image: Uterine anomalies might affect how individuals perceive their bodies and their sense of femininity.
Fertility Struggles: Difficulties in conceiving or maintaining a pregnancy can lead to feelings of frustration, sadness, and disappointment.
Relationship Strain: Couples might experience strain due to the emotional and physical challenges posed by uterine anomalies.
Support Needs: Emotional support from healthcare professionals, support groups, and loved ones can play a crucial role in coping with these challenges.
