
Does a Hysterectomy Remove the Cervix? There are many misconceptions and questions surrounding the topic of hysterectomies, one of the most common being, “Does a hysterectomy remove the cervix?” This is a crucial question, as it influences the aftercare, potential risks, and potential benefits of the procedure. To help you better understand, this comprehensive guide will delve into the specifics of a hysterectomy, its types, the role of the cervix in this procedure, and what to expect during recovery.
Understanding Hysterectomy
A hysterectomy is a surgical procedure that involves the removal of the uterus. It’s one of the most frequently performed gynecological surgeries. The reasons for a hysterectomy can range from uterine fibroids and endometriosis to cancer and chronic pelvic pain1.
Types of Hysterectomy
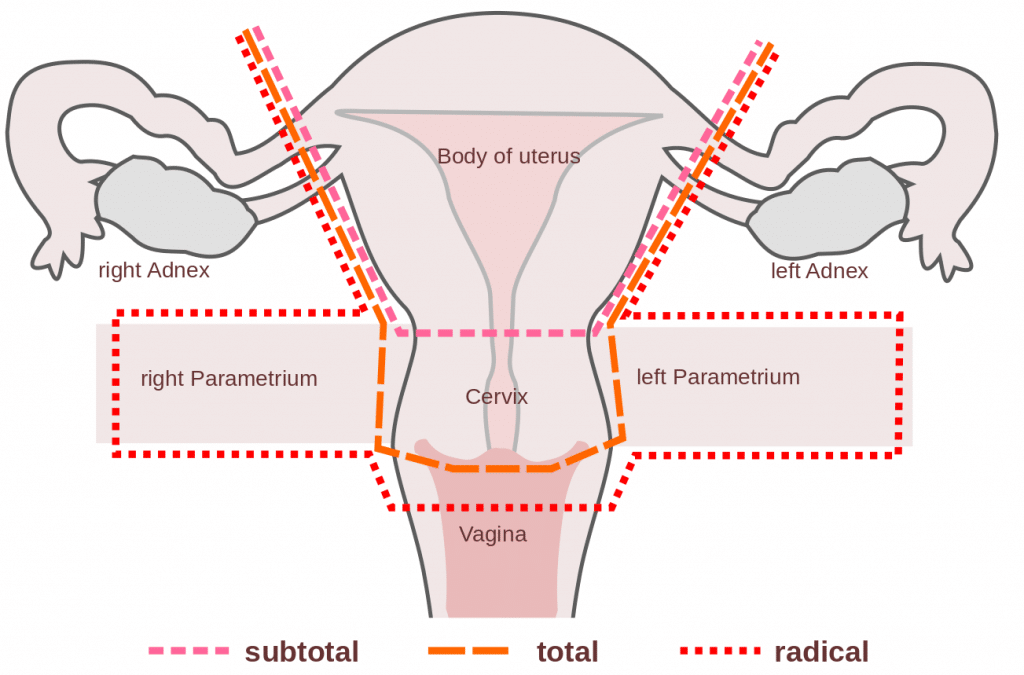
Total Hysterectomy
In a total hysterectomy, both the uterus and the cervix are removed. This is often the preferred option, as removing the cervix eliminates any risk of developing cervical cancer in the future2.
Partial (or Subtotal) Hysterectomy
During a partial hysterectomy, only the uterus is removed, and the cervix is left intact. Research on the benefits and risks of this procedure is ongoing3.
Radical Hysterectomy
A radical hysterectomy is performed when certain cancers are present. This procedure involves removing the whole uterus, tissue on the sides of the uterus, part of the vagina, and occasionally nearby lymph nodes4.
Does a Hysterectomy Always Remove the Cervix?
The removal of the cervix during a hysterectomy depends on the type of hysterectomy being performed. In a total hysterectomy, the cervix is removed along with the uterus. However, in a partial or subtotal hysterectomy, the cervix is left in place5.
Hysterectomy and the Cervix
Whether a hysterectomy involves the removal of the cervix depends on various factors. A hysterectomy is a surgical procedure aimed at removing the uterus, but the decision regarding the cervix varies based on individual circumstances and the type of hysterectomy performed. There are different types of hysterectomies:
- Total Hysterectomy: In a total hysterectomy, both the uterus and the cervix are typically removed. This is the most common type.
- Partial Hysterectomy: A partial hysterectomy involves the removal of the uterus while preserving the cervix. This option may be considered for specific medical conditions.
- Radical Hysterectomy: In cases of advanced cancer, a radical hysterectomy may be performed, which includes the removal of the uterus, cervix, and surrounding tissues.
The decision to remove or preserve the cervix is influenced by the patient’s health, the underlying medical condition, and the surgeon’s expertise. In general, cervix preservation may be preferred in cases where there is no medical necessity for its removal, as it can help maintain natural menstrual cycles and potentially sexual function. However, some medical conditions, such as cervical cancer or precancerous lesions, may require the removal of the cervix to prevent further complications.
It’s crucial for individuals considering a hysterectomy to have a detailed discussion with their healthcare provider to determine the most suitable approach, taking into account their specific medical condition and personal preferences [2][5][10].
Cervical Preservation
Cervical preservation during a hysterectomy is a surgical approach where the cervix is left intact. This is known as a subtotal or partial hysterectomy. Situations in which the cervix might be preserved include:
- Benign Conditions: When a patient has benign gynecological conditions, such as fibroids, endometriosis, or abnormal uterine bleeding, that do not directly involve the cervix, a subtotal hysterectomy may be considered to preserve the cervix [2].
- Patient Choice: Some patients may prefer to retain their cervix, especially if they have concerns about the potential impact of cervix removal on sexual function.
Advantages of preserving the cervix
- Preservation of Sexual Function: Retaining the cervix may help maintain sexual function and pleasure for some women, as the cervix plays a role in sexual response [1].
- Lower Risk of Pelvic Organ Prolapse: Cervical preservation is associated with a reduced risk of pelvic organ prolapse compared to total hysterectomy [4].
Disadvantages of preserving the cervix:
- Cervical Cancer Risk: The cervix remains susceptible to cervical cancer, and regular Pap smears and screenings are still necessary to monitor its health.
- Potential for Residual Symptoms: Some patients may continue to experience symptoms related to the cervix, such as menstrual bleeding if not completely removed during surgery.
The decision to preserve the cervix during a hysterectomy should be made after thorough consultation between the patient and their healthcare provider, taking into consideration the specific medical condition, personal preferences, and potential benefits and risks of the procedure.
Why Might the Cervix Be Left During a Hysterectomy?
In some cases, a woman may prefer to keep her cervix for personal reasons, including sexual function. Some women report a change in their sexual satisfaction after a total hysterectomy, although research findings are mixed. It’s essential to have a thorough discussion with your healthcare provider about the potential risks and benefits before making a decision6.
Benefits of Cervix Removal

Cervix removal, also known as total hysterectomy, can offer several medical benefits in specific situations. It is typically performed in the following medical conditions:
- Cervical Cancer: For individuals diagnosed with cervical cancer or pre-cancerous conditions, removing the cervix is often a crucial part of treatment. It eliminates the source of the disease, reducing the risk of cancer progression and recurrence [3].
- Severe Cervical Dysplasia: In cases of severe cervical dysplasia (precancerous changes in cervical cells), a hysterectomy may be recommended to prevent the development of cervical cancer [3].
- Chronic Cervical Infections: Repeated or severe cervical infections that do not respond to other treatments may necessitate cervical removal to eliminate the source of infection.
- Endometrial or Uterine Conditions: When there are concomitant uterine conditions such as endometriosis or fibroids, a total hysterectomy may be performed to address these issues along with cervical removal.
Cervix removal reduces the risk of cervical cancer primarily because the cervix, which is the primary site for cervical cancer development, is removed. This minimizes the chance of malignant cells forming in the cervix or spreading to other parts of the body. Routine screenings like Pap smears and HPV tests are no longer required after cervix removal, as there is no longer a cervix to screen. However, it’s important to note that regular gynecological check-ups are still necessary for overall health monitoring and well-being.
Risks and Complications
- Cervix removal, often performed during a hysterectomy, is a medical procedure that, like any surgery, carries potential risks and complications. These risks may include infection, bleeding, urinary issues, changes in sexual function, the risk of vaginal vault prolapse, and possible long-term health effects. However, it’s important to note that these complications are relatively rare and often depend on individual factors and surgical techniques [4].
- The importance of informed decision-making cannot be overstated. Patients considering cervix removal should engage in thorough discussions with their healthcare provider, understanding the potential risks and benefits specific to their medical condition. It’s crucial to weigh these factors against the alternatives, including cervical preservation in certain cases. Informed consent empowers individuals to make choices that align with their health goals and preferences. Healthcare professionals should provide comprehensive information, enabling patients to make well-informed decisions that prioritize their overall well-being and quality of life.
Recovery After a Hysterectomy

Recovery times vary depending on the type of hysterectomy performed and the individual’s overall health. In general, hospital stays can range from a day to a week, and total recovery can take anywhere from two to six weeks7.Recovery after a hysterectomy, a surgical procedure to remove the uterus, varies based on the type of hysterectomy performed. Generally, most individuals can expect a recovery period of four to eight weeks, depending on factors such as the surgical approach and individual health. For instance, vaginal or laparoscopic hysterectomies often lead to shorter recovery times, typically around four to six weeks, while abdominal hysterectomies may require six to eight weeks for full recovery [1][2]. During this recovery period, it’s crucial to avoid strenuous activities, sexual intercourse, and heavy lifting, as well as closely follow post-operative care instructions provided by the healthcare provider [6]. It’s important to note that changes in sexual health and well-being can be part of the recovery process, with potential issues such as vaginal dryness or altered libido. Open communication with healthcare providers can address these concerns and explore possible solutions, such as hormone replacement therapy [3].
Generally, post-surgery recovery involves several phases:
- Hospital Stay: Most patients stay in the hospital for a day or two after the surgery, but the duration can be longer depending on the procedure’s complexity and the individual’s health.
- Physical Recovery: Patients typically experience some pain and discomfort, which can be managed with pain medication. It may take several weeks to resume normal activities, and strenuous activities should be avoided during this time [3].
- Sexual Health: After a hysterectomy, some individuals may notice changes in sexual health, such as vaginal dryness or changes in libido. These changes can vary, but it’s essential to communicate with your healthcare provider to address any concerns or explore solutions, such as hormone replacement therapy [3].
- Emotional Well-being: The emotional recovery is an essential aspect of the process. Some individuals may experience mixed emotions, and support from healthcare professionals and loved ones can be valuable in this phase.
- Follow-Up Care: Regular follow-up visits with the healthcare provider are necessary to monitor the healing process and address any complications or concerns.
Recovery after a hysterectomy is a personalized journey, and it’s crucial to follow medical advice and be patient with the healing process. For any concerns about post-surgery changes in sexual health or overall well-being, open and honest communication with the healthcare provider is key to addressing and managing these issues.
Conclusion
Understanding the specifics of a hysterectomy, including whether or not the cervix is removed, can help you make informed decisions about your health. While a total hysterectomy does involve removing the cervix, a partial or subtotal hysterectomy leaves it intact. It’s essential to discuss your options, concerns, and personal circumstances with your healthcare provider to choose the best path forward.
FAQs
Does a hysterectomy always remove the cervix?
No, a hysterectomy doesn’t always remove the cervix. It depends on the type of hysterectomy being performed. A total hysterectomy does remove the cervix, but a partial or subtotal hysterectomy leaves it intact
Why might the cervix be left during a hysterectomy?
In some cases, a woman may prefer to keep her cervix for personal reasons, including sexual function. However, it’s important to discuss this with your healthcare provider, as leaving the cervix can carry a risk of cervical cancer
How long is the recovery period after a hysterectomy?
Recovery times vary depending on the type of hysterectomy performed and the individual’s overall health. In general, hospital stays can range from a day to a week, and total recovery can take anywhere from two to six weeks
Can I still develop cervical cancer if my cervix is left after a hysterectomy?
Yes, there is still a risk of developing cervical cancer if your cervix is left intact after a hysterectomy. Therefore, regular cervical cancer screenings are essential
